Thermography:
- No radiation (Xrays)
- No compression (squeezing)
- No problem with dense or fibrous breasts
- No problem with breast implants
- No problem if pregnant or nursing
- A 15-minute test
- Better able to detect potentially cancerous tissue
- Readings are done by certified MD thermologists
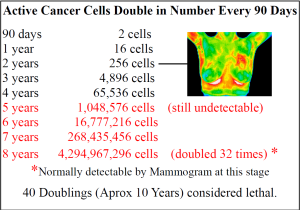
- Cancer cells are typically in the body 10-20 years before the mass gets large enough to be noticed.
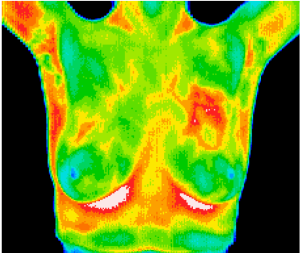
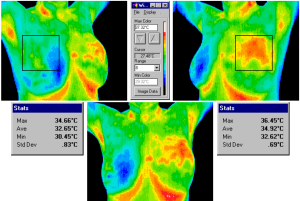
Thermography measures the skin’s autonomic response to that inflammation – its “heat signature.”
The technology converts infrared radiation emitted from the skin surface into electrical impulses that are visualized in color. The spectrum of colors indicates an increase or decrease in the amount of infrared radiation being emitted from the body surface.
Thermography can spot suspicious tissue 10 years before it can be detected by mammography.
Thermography is especially helpful in detecting Inflammatory Breast Disease (IBC). It is rare, but the most aggressive form of breast cancer and has a faster doubling time than other breast cancers. Doubling time is the time it takes for cancer cells to divide and grow. IBC makes up perhaps 3%- 6% of all breast cancers. IBC usually does not manifest as a tumor; it usually grows in nests or “sheets” in the breast. The cancer cells clog the lymph vessels just below the skin giving the classic symptoms of warmth and color changes to the skin. Mammograms and ultrasounds often miss IBC because there is no mass, no tumor. Because IBC has inflammation and heat, thermography is much better at detection.
The consensus among experts is that early detection holds the key to survival. If mammography’s look at structure can detect a cancerous mass, and thermography’s look at systems can detect early suspicions of cancer formation, then it stands to reason thermography can act as an early warning system, giving women the fighting chance they need to win this battle. Thermography is a screening tool which can help raise suspicions of breast cancer at an early stage, when there is still chance of complete cure.
[1] Marilyn A. Roubidoux, MD, Michael S. Sabel, MD, Janet E. Bailey, MD, Celina G. Kleer, MD, Katherine A. Klein, MD and Mark A. Helvie, MD. Small (<2.0-cm) Breast Cancers: Mammographic and US Findings at US-guided Cryoablation—Initial Experience